Wong WL, Su X, Li X, Cheung CMG, Klein R, Cheng CY, et al. International prevalence of age-related macular degeneration and illness burden projection for 2020 and 2040: a scientific evaluate and meta-analysis. Lancet Glob Well being. 2014;2:e106–16.
Heier JS, Lad EM, Holz FG, Rosenfeld PJ, Guymer RH, Boyer D, et al. Pegcetacoplan for the remedy of geographic atrophy secondary to age-related macular degeneration (OAKS and DERBY): two multicentre, randomised, double-masked, sham-controlled, section 3 trials. Lancet. 2023;402:1434–48.
Khanani AM, Patel SS, Staurenghi G, Tadayoni R, Danzig CJ, Eichenbaum DA, et al. Efficacy and security of avacincaptad pegol in sufferers with geographic atrophy (GATHER2): 12-month outcomes from a randomised, double-masked, section 3 trial. Lancet. 2023;402:1449–58.
Chakravarthy U, Bailey CC, Scanlon PH, McKibbin M, Khan RS, Mahmood S, et al. Progression from early/intermediate to superior types of age-related macular degeneration in a big UK cohort: charges and threat elements. Ophthalmol Retin. 2020;4:662–72.
Vogl WD, Riedl S, Mai J, Reiter GS, Lachinov D, Bogunović H, et al. Predicting topographic illness progression and remedy response of pegcetacoplan in geographic atrophy quantified by deep studying. Ophthalmol Retin. 2023;7:4–13.
Heier JS, Khanani AM, Quezada Ruiz C, Basu Okay, Ferrone PJ, Brittain C, et al. Efficacy, sturdiness, and security of intravitreal faricimab as much as each 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): two randomised, double-masked, section 3, non-inferiority trials. Lancet. 2022;399:729–40.
Fujimoto J, Swanson E. The event, commercialization, and impression of optical coherence tomography. Investig Ophthalmol Vis Sci. 2016;57:OCT1–13.
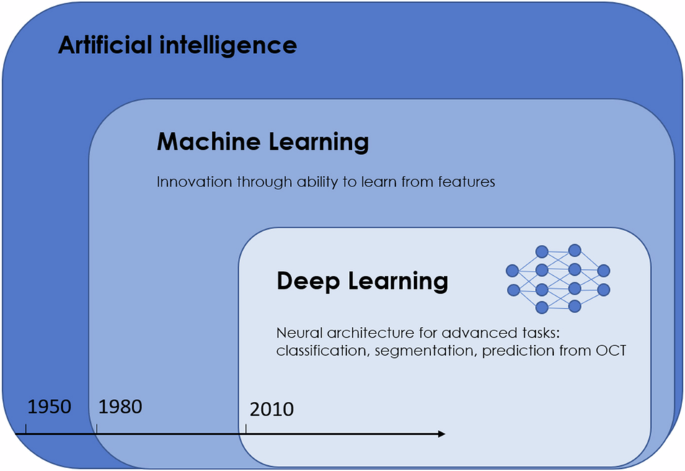
Schmidt-Erfurth U, Sadeghipour A, Gerendas BS, Waldstein SM, Bogunović H. Artificial intelligence in retina. Prog Retin Eye Res. 2018;67:1–29.
Burlina PM, Joshi N, Pekala M, Pacheco KD, Freund DE, Bressler NM. Automated grading of age-related macular degeneration from shade fundus photographs utilizing deep convolutional neural networks. JAMA Ophthalmol. 2017;135:1170–6.
Treder M, Lauermann JL, Eter N. Automated detection of exudative age-related macular degeneration in spectral area optical coherence tomography utilizing deep studying. Graefes Arch Clin Exp Ophthalmol. 2018;256:259–65.
Treder M, Lauermann JL, Eter N. Deep learning-based detection and classification of geographic atrophy utilizing a deep convolutional neural community classifier. Graefes Arch Clin Exp Ophthalmol. 2018;256:2053–60. https://doi.org/10.1007/S00417-018-4098-2.
Pontikos N, Woof W, Veturi A, Javanmardi B, Ibarra-Arellano M, Hustinx A, et al. Eye2Gene: prediction of causal inherited retinal illness gene from multimodal imaging utilizing deep-learning n.d. https://doi.org/10.21203/rs.3.rs-2110140/v1.
Saksens NTM, Fleckenstein M, Schmitz-Valckenberg S, Holz FG, den Hollander AI, Keunen JEE, et al. Macular dystrophies mimicking age-related macular degeneration. Prog Retin Eye Res. 2014;39:23–57.
Orlando JI, Gerendas BS, Riedl S, Grechenig C, Breger A, Ehler M, et al. Automated quantification of photoreceptor alteration in macular illness utilizing optical coherence tomography and deep studying. Sci Rep. https://doi.org/10.1038/s41598-020-62329-9.
Garvin MK, Abràmoff MD, Kardon R, Russell SR, Wu X, Sonka M. Intraretinal layer segmentation of macular optical coherence tomography photographs utilizing optimum 3-D graph search. IEEE Trans Med Imaging. 2008;27:1495–505.
Chen YM, Huang WT, Ho WH, Tsai JT. Classification of age-related macular degeneration utilizing convolutional-neural-network-based switch studying. BMC Bioinforma. 2021;22:1–16.
Zhou Y, Chia MA, Wagner SK, Ayhan MS, Williamson DJ, Struyven RR, et al. A basis mannequin for generalizable illness detection from retinal photographs. Nature. 2023;622:156–63. 2023;622:156–63.
Hochreiter S, Schmidhuber J. Lengthy short-term reminiscence. Neural Comput. 1997;9:1735–80.
Schlegl T, Seeböck P, Waldstein SM, Langs G, Schmidt-Erfurth U. f-AnoGAN: quick unsupervised anomaly detection with generative adversarial networks. Med Picture Anal. 2019;54:30–44.
Kugelman J, Alonso-Caneiro D, Learn SA, Collins MJ. A evaluate of generative adversarial community functions in optical coherence tomography picture evaluation. J Optom. 2022;15:S1–11.
Ferris FL, Wilkinson CP, Hen A, Chakravarthy U, Chew E, Csaky Okay, et al. Scientific classification of age-related macular degeneration. Ophthalmology. 2013;120:844–51.
Bogunović H, Montuoro A, Baratsits M, Karantonis MG, Waldstein SM, Schlanitz F, et al. Machine studying of the progression of intermediate age-related macular degeneration based mostly on OCT imaging. Make investments Ophthalmol Vis Sci. 2017;58:BIO141–50.
Chen M, Jin Okay, Yan Y, Liu X, Huang X, Gao Z, et al. Automated analysis of age-related macular degeneration utilizing multi-modal vertical airplane characteristic fusion through deep studying. Med Phys. 2022;49:2324–33.
Saßmannshausen M, Steinberg JS, Fimmers R, Pfau M, Thiele S, Fleckenstein M, et al. Construction-function evaluation in sufferers with intermediate age-related macular degeneration. Make investments Ophthalmol Vis Sci. 2018;59:1599–608.
Guymer RH, Brassington KH, Dimitrov P, Makeyeva G, Plunkett M, Xia W, et al. Nanosecond-laser software in intermediate AMD: 12-month outcomes of fundus look and macular perform. Clin Exp Ophthalmol. 2014;42:466–79.
Robinson DG, Margrain TH, Dunn MJ, Bailey C, Binns AM. Low-level nighttime gentle remedy for age-related macular degeneration: a randomized medical trial. Make investments Ophthalmol Vis Sci. 2018;59:4531–41.
Finger RP, Schmitz-Valckenberg S, Schmid M, Rubin GS, Dunbar H, Tufail A, et al. MACUSTAR: growth and medical validation of purposeful, structural, and patient-reported endpoints in intermediate age-related macular degeneration. Ophthalmologica. 2019;241:61–72.
Sutton J, Menten MJ, Riedl S, Bogunović H, Leingang O, Anders P, et al. Creating and validating a multivariable prediction mannequin which predicts progression of intermediate to late age-related macular degeneration—the PINNACLE trial protocol. Eye. 2022;37:6. 2022;37:1275–83.
Ferrara D, Silver RE, Louzada RN, Novais EA, Collins GK, Seddon JM. Optical coherence tomography options previous the onset of superior age-related macular degeneration. Investig Ophthalmol Vis Sci. 2017;58:3519.
Marsiglia M, Boddu S, Bearelly S, Xu L, Breaux BE, Freund KB, et al. Affiliation between geographic atrophy progression and reticular pseudodrusen in eyes with dry age-related macular degeneration. Investig Ophthalmol Vis Sci. 2013;54:7362–9.
Reiter GS, Informed R, Schranz M, Baumann L, Mylonas G, Sacu S, et al. Subretinal drusenoid deposits and photoreceptor loss detecting international and native progression of geographic atrophy by SD-OCT imaging. Investig Ophthalmol Vis Sci. 2020;61:11–11.
Niu S, Sisternes L. Totally automated prediction of geographic atrophy progress utilizing quantitative spectral-domain optical coherence tomography biomarkers. Ophthalmology. 2016;123:1737–50.
Pfau M, Von Der Emde L, De Sisternes L, Hallak JA, Leng T, Schmitz-Valckenberg S, et al. Progression of photoreceptor degeneration in geographic atrophy secondary to age-related macular degeneration. JAMA Ophthalmol. 2020;138:1026–34.
Guymer RH, Rosenfeld PJ, Curcio CA, Holz FG, Staurenghi G, Freund KB, et al. Incomplete retinal pigment epithelial and outer retinal atrophy (iRORA) in age-related macular degeneration: CAM report 4. Ophthalmology. 2020;127:394.
Zadeh SG, Wintergerst MWM, Wiens V, Thiele S, Holz FG, Finger RP, et al. CNNs allow correct and quick segmentation of drusen in optical coherence tomography. In: Cardoso, M., et al. Deep studying in medical picture evaluation and multimodal studying for medical resolution help. DLMIA ML-CDS 2017 2017. Lecture Notes in Laptop Science(), vol 10553. Springer, Cham. https://doi.org/10.1007/978-3-319-67558-9_8.
Schuman SG, Koreishi AF, Farsiu S, Jung SH, Izatt JA, Toth CA. Photoreceptor layer thinning over drusen in eyes with age-related macular degeneration imaged in vivo with spectral-domain optical coherence tomography. Ophthalmology. 2009;116:488–.e2. https://doi.org/10.1016/J.OPHTHA.2008.10.006.
Sevilla MB, McGwin G, Lad EM, Clark M, Yuan EL, Farsiu S, et al. Relating retinal morphology and performance in getting old and early to intermediate age-related macular degeneration topics. Am J Ophthalmol. 2016;165:65–77.
Saßmannshausen M, Behning C, Isselmann B, Schmid M, Finger RP, Holz FG, et al. Relative ellipsoid zone reflectivity and its affiliation with illness severity in age-related macular degeneration: a MACUSTAR research report. Sci Rep. 2022;12:14933. 2022;12:1–12.
Orlando JI, Gerendas BS, Riedl S, Grechenig C, Breger A, Ehler M, et al. Automated quantification of photoreceptor alteration in macular illness utilizing optical coherence tomography and deep studying. Sci Rep. 2020;10:5619. 2020;10:1–12.
Kalra G, Cetin H, Whitney J, Yordi S, Cakir Y, McConville C, et al. Automated identification and segmentation of ellipsoid zone at-risk utilizing deep studying on SD-OCT for predicting progression in dry AMD. Diagnostics. 2023;13:1178 https://doi.org/10.3390/DIAGNOSTICS13061178.
Lu J, Cheng Y, Hiya FE, Shen M, Herrera G, Zhang Q, et al. Deep-learning-based automated measurement of outer retinal layer thickness to be used in the evaluation of age-related macular degeneration, relevant to each swept-source and spectral-domain OCT imaging. Biomed Choose Categorical. 2023;15:413.
Riedl S, Schmidt-Erfurth U, Rivail A, Birner Okay, Mai J, Vogl WD, et al. Sequence of morphological adjustments previous atrophy in intermediate AMD utilizing deep studying. Investig Ophthalmol Vis Sci. 2024;65:30–30.
Li M, Dolz-Marco R, Huisingh C, Messinger JD, Feist RM, Ferrara D, et al. Clinicopathologic correlation of geographic atrophy secondary to age-related macular degeneration. Retina. 2019;39:802 https://doi.org/10.1097/IAE.0000000000002461.
Zanzottera EC, Ach T, Huisingh C, Messinger JD, Spaide RF, Curcio CA. VIsualizing retinal pigment epithelium phenotypes in the transition to geographic atrophy in age-related macular degeneration. Retina. 2016;36:S12–25.
Nassisi M, Fan W, Shi Y, Lei J, Borrelli E, Ip M, et al. Amount of intraretinal hyperreflective foci in sufferers with intermediate age-related macular degeneration correlates with 1-year progression. Investig Ophthalmol Vis Sci. 2018;59:3431–9.
Schlegl T, Bogunovic H, Klimscha S, Seeböck P, Sadeghipour A, Gerendas B, et al. Totally automated segmentation of hyperreflective foci in optical coherence tomography photographs. 2018.
Schmidt-Erfurth U, Bogunovic H, Grechenig C, Bui P, Fabianska M, Waldstein S, et al. Position of deep learning-quantified hyperreflective foci for the prediction of geographic atrophy progression. Am J Ophthalmol. 2020;216:257–70.
Finger RP, Wu Z, Luu CD, Kearney F, Ayton LN, Lucci LM, et al. Reticular pseudodrusen: a threat issue for geographic atrophy in fellow eyes of people with unilateral choroidal neovascularization. Ophthalmology. 2014;121:1252–6.
Van Grinsven MJJP, Brussee C, Ginneken BVan, Buitendijk GHS, Hoyng CB, Theelen T. et al. Computerized identification of reticular pseudodrusen utilizing multimodal retinal picture evaluation. Investig Ophthalmol Vis Sci. 2015;56:633–9.
Wu Z, Schmitz-Valckenberg S, Blodi BA, Holz FG, Jaffe GJ, Liakopoulos S, et al. Reticular pseudodrusen: interreader settlement of analysis on OCT imaging in age-related macular degeneration. Ophthalmol Sci. 2023;3:100325.
Schwartz R, Khalid H, Liakopoulos S, Ouyang Y, de Vente C, González-Gonzalo C, et al. A deep studying framework for the detection and quantification of reticular pseudodrusen and drusen on optical coherence tomography. Transl Vis Sci Technol. 2022;11:3–3.
Mishra Z, Ganegoda A, Selicha J, Wang Z, Sadda SVR, Hu Z. Automated retinal layer segmentation utilizing graph-based algorithm incorporating deep-learning-derived info. Sci Rep. 2020;10:9541.
Heesterbeek TJ, Lorés-Motta L, Hoyng CB, Lechanteur YTE, den Hollander AI. Threat elements for progression of age-related macular degeneration. Ophthalmic Physiol Choose. 2020;40:140–70.
Schlanitz FG, Baumann B, Kundi M, Sacu S, Baratsits M, Scheschy U, et al. Drusen quantity growth over time and its relevance to the course of age-related macular degeneration. Br J Ophthalmol. 2017;101:198–203.
Wu Z, Luu CD, Ayton LN, Goh JK, Lucci LM, Hubbard WC, et al. Optical coherence tomography-defined adjustments previous the event of drusen-associated atrophy in age-related macular degeneration. Ophthalmology. 2014;121:2415–22.
Garzone D, Terheyden JH, Morelle O, Wintergerst MWM, Saßmannshausen M, Schmitz-Valckenberg S, et al. Comparability of automated drusen quantity measurements in age-related macular degeneration: a MACUSTAR research report. Sci Rep. 2022;12:21911. 2022;12:1–10.
Vogl WD, Bogunović H, Waldstein SM, Riedl S, Schmidt-Erfurth U. Spatio-temporal alterations in retinal and choroidal layers in the progression of age-related macular degeneration (AMD) in optical coherence tomography. Sci Rep. 2021;11:5743. 2021;11:1–11.
Leingang O, Riedl S, Mai J, Reiter GS, Faustmann G, Fuchs P, et al. Automated deep learning-based AMD detection and staging in real-world OCT datasets (PINNACLE research report 5). Sci Rep. 2023;13:19545 https://doi.org/10.1038/S41598-023-46626-7.
Schmidt-Erfurth U, Waldstein SM, Klimscha S, Sadeghipour A, Hu X, Gerendas BS, et al. Prediction of particular person illness conversion in early AMD utilizing synthetic intelligence. Make investments Ophthalmol Vis Sci. 2018;59:3199–208.
Lad EM, Sleiman Okay, Banks DL, Hariharan S, Clemons T, Herrmann R, et al. Machine studying OCT predictors of progression from intermediate age-related macular degeneration to geographic atrophy and imaginative and prescient loss. Ophthalmol Sci. 2022;2:100160 https://doi.org/10.1016/J.XOPS.2022.100160.
Burlina PM, Joshi N, Pacheco KD, Freund DE, Kong J, Bressler NM. Use of deep studying for detailed severity characterization and estimation of 5-year threat amongst sufferers with age-related macular degeneration. JAMA Ophthalmol. 2018;136:1359.
Peng Y, Keenan TD, Chen Q, Agrón E, Allot A, Wong WT, et al. Predicting threat of late age-related macular degeneration utilizing deep studying. npj Digit Med. 2020;3:111. 2020;3:1–10.
Ajana S, Cougnard-Grégoire A, Colijn JM, Merle BMJ, Verzijden T, de Jong PTVM. et al. Predicting progression to superior age-related macular degeneration from medical, genetic, and life-style elements utilizing machine studying. Ophthalmology. 2021;128:587–97.
Banerjee I, de Sisternes L, Hallak JA, Leng T, Osborne A, Rosenfeld PJ, et al. Prediction of age-related macular degeneration illness utilizing a sequential deep studying method on longitudinal SD-OCT imaging biomarkers. Sci Rep. 2020;10:15434. 2020 10:1
Dow ER, Jeong HK, Katz EA, Toth CA, Wang D, Lee T, et al. A deep-learning algorithm to foretell short-term progression to geographic atrophy on spectral-domain optical coherence tomography. JAMA Ophthalmol. 2023;141:1052–61.
Li M, Huisingh C, Messinger J, Dolz-Marco R, Ferrara D, Bailey Freund Okay, et al. Histology of geographic atrophy secondary to age-related macular degeneration: a multilayer method. Retina. 2018;38:1937–53.
Wu Z, Luu CD, Ayton LN, Goh JK, Lucci LM, Hubbard WC, et al. Fundus autofluorescence traits of nascent geographic atrophy in age-related macular degeneration. Investig Ophthalmol Vis Sci. 2015;56:1546–52.
Schmitz-Valckenberg S, Sahel JA, Danis R, Fleckenstein M, Jaffe GJ, Wolf S, et al. Pure historical past of geographic atrophy progression secondary to age-related macular degeneration (geographic atrophy progression research). Ophthalmology. 2016;123:361–8.
Schmitz-Valckenberg S, Fleckenstein M, Scholl HPN, Holz FG. Fundus autofluorescence and progression of age-related macular degeneration. Surv Ophthalmol. 2009;54:96–117.
Schmitz-Valckenberg S, Jorzik J, Unnebrink Okay, Holz FG. Evaluation of digital scanning laser ophthalmoscopy fundus autofluorescence photographs of geographic atrophy in superior age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2002;240:73–8.
Spaide T, Jiang J, Patil J, Anegondi N, Steffen V, Kawczynski MG, et al. Geographic atrophy segmentation utilizing multimodal deep studying. Transl Vis Sci Technol. 2023;12:10–10.
Arslan J, Samarasinghe G, Sowmya A, Benke KK, Hodgson LAB, Guymer RH, et al. Deep studying utilized to automated segmentation of geographic atrophy in fundus autofluorescence photographs. Transl Vis Sci Technol. 2021;10:2–2.
Anegondi N, Gao SS, Steffen V, Spaide RF, Sadda SVR, Holz FG, et al. Deep studying to foretell geographic atrophy space and progress fee from multimodal imaging. Ophthalmol Retin. 2023;7:243–52.
Schmitz-Valckenberg S, Brinkmann CK, Alten F, Herrmann P, Stratmann NK, Göbel AP, et al. Semiautomated picture processing methodology for identification and quantification of geographic atrophy in age-related macular degeneration. Investig Ophthalmol Vis Sci. 2011;52:7640–6.
Fleckenstein M, Mitchell P, Freund KB, Sadda S, Holz FG, Brittain C, et al. The progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2017. https://doi.org/10.1016/j.ophtha.2017.08.038.
Pilotto E, Benetti E, Convento E, Guidolin F, Longhin E, Parrozzani R, et al. Microperimetry, fundus autofluorescence, and retinal layer adjustments in progressing geographic atrophy. Can J Ophthalmol. 2013;48:386–93.
Pilotto E, Guidolin F, Convento E, Spedicato L, Vujosevic S, Cavarzeran F, et al. Fundus autofluorescence and microperimetry in progressing geographic atrophy secondary to age-related macular degeneration. Br J Ophthalmol. 2013;97:622–6.
Sadda SR, Chakravarthy U, Birch DG, Staurenghi G, Henry EC, Brittain C. Scientific endpoints for the research of geographic atrophy secondary to age-related macular degeneration. Retina. 2016;36:1806.
Holz FG, Sadda SVR, Staurenghi G, Lindner M, Hen AC, Blodi BA, et al. Imaging protocols in medical research in superior age-related macular degeneration: suggestions from classification of atrophy consensus conferences. Ophthalmology. 2017;124:464–78.
Holz FG, Bindewald-Wittich A, Fleckenstein M, Dreyhaupt J, Scholl HPN, Schmitz-Valckenberg S. Progression of geographic atrophy and impression of fundus autofluorescence patterns in age-related macular degeneration. Am J Ophthalmol. 2007;143:463–72. https://doi.org/10.1016/J.AJO.2006.11.041.
Deckert A, Schmitz-Valckenberg S, Jorzik J, Bindewald A, Holz FG, Mansmann U. Automated evaluation of digital fundus autofluorescence photographs of geographic atrophy in superior age-related macular degeneration utilizing confocal scanning laser ophthalmoscopy (cSLO). BMC Ophthalmol. 2005;5:8.
Fleckenstein M, Adrion C, Valckenberg SS, Göbel AP, Wittich AB, Scholl HPN, et al. Concordance of illness progression in bilateral geographic atrophy because of AMD. Investig Ophthalmol Vis Sci. 2010;51:637–42.
Hu Z, Medioni GG, Hernandez M, Sadda SR. Automated segmentation of geographic atrophy in fundus autofluorescence photographs utilizing supervised pixel classification. J Med Imaging. 2015;2:014501.
Riedl S, Vogl WD, Mai J, Reiter GS, Lachinov D, Grechenig C, et al. The impact of pegcetacoplan remedy on photoreceptor upkeep in geographic atrophy monitored by synthetic intelligence-based OCT evaluation. Ophthalmol Retin. 2022;6:1009–18.
Bui PTA, Reiter GS, Fabianska M, Waldstein SM, Grechenig C, Bogunovic H, et al. Fundus autofluorescence and optical coherence tomography biomarkers related to the progression of geographic atrophy secondary to age-related macular degeneration. Eye. 2022;36:2013–9.
Pfau M, Lindner M, Goerdt L, Thiele S, Nadal J, Schmid M, et al. Prognostic worth of shape-descriptive elements for the progression of geographic atrophy secondary to age-related macular degeneration. Retina. 2019;39:1527–39.
Mai J, Riedl S, Reiter GS, Lachinov D, Vogl W-D, Bogunovic H, et al. Comparability of FAF versus OCT-based analysis of the therapeutic response to pegcetacoplan in geographic atrophy. Am J Ophthalmol. 2022. https://doi.org/10.1016/J.AJO.2022.06.023.
Romond Okay, Alam M, Kravets S, Sisternes L, de, Leng T, Lim JI, et al. Imaging and synthetic intelligence for progression of age-related macular degeneration. Exp Biol Med. 2021;246:2159–69.
Wu Z, Terheyden JH, Hodgson LAB, Guymer RH. Choroidal sign hypertransmission on optical coherence tomography imaging: affiliation with growth of geographic atrophy in age-related macular degeneration. Clin Exp Ophthalmol. 2024. https://doi.org/10.1111/CEO.14356.
Pramil V, de Sisternes L, Omlor L, Lewis W, Sheikh H, Chu Z, et al. A deep studying mannequin for automated segmentation of geographic atrophy imaged utilizing swept-source OCT. Ophthalmol Retin. 2023;7:127–41.
Litts KM, Zhang Y, Bailey Freund Okay, Curcio CA. Optical coherence tomography and histology of age-related macular degeneration help mitochondria as reflectivity sources. Retina. 2018;38:445.
Vujosevic S, Loewenstein A, O’Toole L, Schmidt-Erfurth UM, Zur D, Chakravarthy U. Imaging geographic atrophy: integrating construction and performance to raised perceive the consequences of new therapies. Br J Ophthalmol. 2024. https://doi.org/10.1136/BJO-2023-324246.
Holz FG, Strauss EC, Schmitz-Valckenberg S, Van Lookeren Campagne M. Geographic atrophy: medical options and potential therapeutic approaches. Ophthalmology. 2014;121:1079–91.
Landa G, Su E, Garcia PMT, Seiple WH, Rosen RB. Interior segment-outer section junctional layer integrity and corresponding retinal sensitivity in dry and moist types of age-related macular degeneration. Retina. 2011;31:364–70.
Lachinov, D., Seeböck, P., Mai, J., Goldbach, F., Schmidt-Erfurth, U., Bogunovic, H. (2021). Projective Skip-Connections for Segmentation Alongside a Subset of Dimensions in Retinal OCT. In: de Bruijne, M., et al. Medical Picture Computing and Laptop Assisted Intervention – MICCAI 2021. MICCAI 2021. Lecture Notes in Laptop Science(), vol 12901. Springer, Cham. https://doi.org/10.1007/978-3-030-87193-2_41.
Gass, J. D. Stereoscopic Atlas of Macular Ailments Analysis and Remedy (Mosby-Yr E book Inc., 1977).
Spaide RF, Jaffe GJ, Sarraf D, Freund KB, Sadda SR, Staurenghi G, et al. Consensus nomenclature for reporting neovascular age-related macular degeneration information: consensus on neovascular age-related macular degeneration nomenclature research group. Ophthalmology. 2020;127:616–36.
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1432–44.
Schmidt-Erfurth U, Chong V, Loewenstein A, Larsen M, Souied E, Schlingemann R, et al. Pointers for the administration of neovascular age-related macular degeneration by the European Society of Retina Specialists (EURETINA). Br J Ophthalmol. 2014;98:1144–67.
Fileta JB, Scott IU, Flynn HW. Meta-analysis of infectious endophthalmitis after intravitreal injection of anti-vascular endothelial progress issue brokers. Ophthalmic Surg Lasers Imaging Retina. 2014;45:143–9.
Modi YS, Tanchon C, Ehlers JP. Comparative security and tolerability of anti-VEGF remedy in age-related macular degeneration. Drug Saf. 2015;38:279–93.
Fung AE, Lalwani GA, Rosenfeld PJ, Dubovy SR, Michels S, Feuer WJ, et al. An optical coherence tomography-guided, variable dosing routine with intravitreal ranibizumab (Lucentis) for neovascular age-related macular degeneration. Am J Ophthalmol. 2007;143:566–83. https://doi.org/10.1016/J.AJO.2007.01.028.
Abedi F, Wickremasinghe S, Islam AFM, Inglis KM, Guymer RH. Anti-VEGF remedy in neovascular age-related macular degeneration: a treat-and-extend protocol over 2 years. Retina. 2014;34:1531–8.
Okada M, Mitchell P, Finger RP, Eldem B, Talks SJ, Hirst C, et al. Nonadherence or nonpersistence to intravitreal injection remedy for neovascular age-related macular degeneration: a mixed-methods systematic evaluate. Ophthalmology. 2021;128:234–47.
Khanani AM, Skelly A, Bezlyak V, Griner R, Torres LR, Sagkriotis A. SIERRA-AMD: a retrospective, real-world proof research of sufferers with neovascular age-related macular degeneration in america. Ophthalmol Retin. 2020;4:122–33.
Simader C, Ritter M, Bolz M, Deák GG, Mayr-Sponer U, Golbaz I, et al. Morphologic parameters related for visible consequence throughout anti-angiogenic remedy of neovascular age-related macular degeneration. Ophthalmology. 2014;121:1237–45.
Daniel E, Toth CA, Grunwald JE, Jaffe GJ, Martin DF, Fantastic SL, et al. Threat of scar in the comparability of age-related macular degeneration therapies trials. Ophthalmology. 2014;121:656–66.
Romano F, Cozzi E, Airaldi M, Nassisi M, Viola F, Aretti A, et al. Ten-year incidence of fibrosis and threat elements for its growth in neovascular age-related macular degeneration. Am J Ophthalmol. 2023;252:170–81.
Waldstein SM, Philip AM, Leitner R, Simader C, Langs G, Gerendas BS, et al. Correlation of 3-dimensionally quantified intraretinal and subretinal fluid with visible acuity in neovascular age-related macular degeneration. JAMA Ophthalmol. 2016;134:182–90.
Chakravarthy U, Goldenberg D, Younger G, Havilio M, Rafaeli O, Benyamini G, et al. Automated identification of lesion exercise in neovascular age-related macular degeneration. Ophthalmology. 2016;123:1731–6.
De Fauw J, Ledsam JR, Romera-Paredes B, Nikolov S, Tomasev N, Blackwell S, et al. Clinically relevant deep studying for analysis and referral in retinal illness. Nat Med. 2018;24:9. 2018;24:1342–50
Schlegl T, Waldstein SM, Bogunovic H, Endstraßer F, Sadeghipour A, Philip AM, et al. Totally automated detection and quantification of macular fluid in OCT utilizing deep studying. Ophthalmology. 2018;125:549–58.
Gerendas BS, Sadeghipour A, Michl M, Goldbach F, Mylonas G, Gruber A, et al. Validation of an automatic fluid algorithm on real-world information of neovascular age-related macular degeneration over 5 years. Retina. 2022;42:1673–82.
Martin-Pinardel R, Izquierdo-Serra J, De Zanet S, Parrado-Carrillo A, Garay-Aramburu G, Puzo M, et al. Artificial intelligence-based fluid quantification and related visible outcomes in a real-world, multicentre neovascular age-related macular degeneration nationwide database. Br J Ophthalmol. 2023;108:253–62.
Wilson M, Chopra R, Wilson MZ, Cooper C, MacWilliams P, Liu Y, et al. Validation and medical applicability of whole-volume automated segmentation of optical coherence tomography in retinal illness utilizing deep studying. JAMA Ophthalmol. 2021;139:964–73.
Liu Y, Holekamp NM, Heier JSProspective. Longitudinal research: every day self-imaging with house OCT for neovascular age-related macular degeneration. Ophthalmol Retin. 2022;6:575–85.
Keenan TDL, Loewenstein A. Artificial intelligence for house monitoring gadgets. Curr Opin Ophthalmol. 2023;34:441–8.
Schmidt-Erfurth U, Vogl WD, Jampol LM, Bogunović H. Utility of automated quantification of fluid volumes to anti–VEGF remedy of neovascular age-related macular degeneration. Ophthalmology. 2020;127:1211–9.
Moraes G, Fu DJ, Wilson M, Khalid H, Wagner SK, Korot E, et al. Quantitative evaluation of OCT for neovascular age-related macular degeneration utilizing deep studying. Ophthalmology. 2021;128:693–705.
Schmidt-Erfurth U, Mulyukov Z, Gerendas BS, Reiter GS, Lorand D, Weissgerber G, et al. Therapeutic response in the HAWK and HARRIER trials utilizing deep studying in retinal fluid quantity and compartment evaluation. Eye. 2022. https://doi.org/10.1038/S41433-022-02077-4.
Sharma S, Toth CA, Daniel E, Grunwald JE, Maguire MG, Ying GS, et al. Macular morphology and visible acuity in the second 12 months of the comparability of age-related macular degeneration therapies trials. Ophthalmology. 2016;123:865–75.
Chakravarthy U, Havilio M, Syntosi A, Pillai N, Wilkes E, Benyamini G, et al. Impression of macular fluid quantity fluctuations on visible acuity throughout anti-VEGF remedy in eyes with nAMD. Eye. 2021;35:11. 2021;35:2983–90
Ehlers JP, Zahid R, Kaiser PK, Heier JS, Brown DM, Meng X, et al. Longitudinal evaluation of ellipsoid zone integrity, subretinal hyperreflective materials, and subretinal pigment epithelium illness in neovascular age-related macular degeneration. Ophthalmol Retin. 2021;5:1204–13.
Reiter GS, Mares V, Leingang O, Fuchs P, Bogunovic H, Barthelmes D, et al. Lengthy-term impact of fluid volumes throughout the upkeep section in neovascular age-related macular degeneration: outcomes from Combat Retinal Blindness! Can J Ophthalmol. 2023;0. https://doi.org/10.1016/j.jcjo.2023.10.017.
Schmidt-Erfurth U, Bogunovic H, Sadeghipour A, Schlegl T, Langs G, Gerendas BS, et al. Machine studying to investigate the prognostic worth of present imaging biomarkers in neovascular age-related macular degeneration. Ophthalmol Retin. 2018;2:24–30.
Fu DJ, Faes L, Wagner SK, Moraes G, Chopra R, Patel PJ, et al. Predicting incremental and future visible change in neovascular age-related macular degeneration utilizing deep studying. Ophthalmol Retin. 2021;5:1074–84. https://doi.org/10.1016/J.ORET.2021.01.009.
Romo-Bucheli D, Erfurth US, Bogunovic H. Finish-to-end deep studying mannequin for predicting remedy necessities in neovascular amd from longitudinal retinal OCT imaging. IEEE J Biomed Well being Inf. 2020;24:3456–65.
Mares V, Schmidt-Erfurth UM, Leingang O, Fuchs P, Nehemy MB, Bogunovic H, et al. Authorised AI-based fluid monitoring to establish morphological and purposeful remedy outcomes in neovascular age-related macular degeneration in real-world routine (FRB!). Br J Ophthalmol 2023. https://doi.org/10.1136/BJO-2022-323014.
Liu Y, Yang J, Zhou Y, Wang W, Zhao J, Yu W, et al. Prediction of OCT photographs of short-term response to anti-VEGF remedy for neovascular age-related macular degeneration utilizing generative adversarial community. Br J Ophthalmol. 2020;104:1735–40.
Ting DSW, Peng L, Varadarajan AV, Keane PA, Burlina PM, Chiang MF, et al. Deep studying in ophthalmology: the technical and medical issues. Prog Retin Eye Res. 2019;72:100759 https://doi.org/10.1016/J.PRETEYERES.2019.04.003.